Therapies for Mitochondrial Disease – Past, Present, and Future
Science moves fastest when everyone can take part. That’s why MitoCanada is committed to empowering our community with knowledge. By translating cutting-edge mitochondrial research into clear, easy-to-understand summaries, we aim to nurture curiosity, strengthen understanding, and build confidence in the science driving hope and progress.
Lay Summary: Therapies for Mitochondrial Disease – Past, Present, and Future
Authors:
Ball, M., van Bergen, N.J., Compton, A.G., Thorburn, D.R., Rahman, S., & Christodoulou, J. (2025). Therapies for Mitochondrial Disease: Past, Present, and Future. Journal of Inherited Metabolic Disease, 48:e70065.
What’s this research about?
This review examines how treatments for mitochondrial disease (MD) have evolved over the past six decades, and where the field is heading next. The authors trace the journey from the first clinical description of mitochondrial dysfunction in the early 1960s to today’s rapidly expanding era of genetic discovery and targeted therapeutics.
The review explores both the current management strategies for specific mitochondrial diseases (like CoQ10, thiamine, biotin, and exercise) and the emerging therapeutic frontiers, including dietary approaches, gene and RNA-based therapies, small molecule treatments, and mitochondrial-targeted peptides. It also critically discusses why translating scientific breakthroughs into effective clinical treatments remains challenging, a reflection of the biological complexity and variability of mitochondrial disorders.
Why is this important?
For decades, families affected by mitochondrial disease have faced a difficult reality: although diagnosis has improved, effective treatments remain limited. This review highlights the steady progress being made to change that. The field is shifting from supportive care toward precision medicine, treatments designed to correct the root causes of mitochondrial dysfunction rather than just relieve symptoms.
The authors also discuss why turning scientific discoveries into real treatments is so challenging. Mitochondrial diseases are rare, caused by many different genetic changes, and can look very different from one person to another. It’s also hard to get treatments to reach energy-hungry organs like the brain and heart, where they’re needed most. Researchers are still working to find reliable ways to measure whether a therapy is truly helping, both through biomarkers (measurable signs in the body that show how the disease is behaving) and outcome measures (tests or observations that show whether a treatment is improving health or quality of life).
Even with these challenges, the review makes it clear that mitochondrial medicine is moving forward faster than ever, powered by international teamwork, strong patient involvement, and innovative clinical trial design.
How did they study this?
Instead of focusing on one experiment, the authors brought together decades of research to paint a clear picture of where mitochondrial medicine stands today. They reviewed scientific papers, clinical trial results, and case studies that explored everything from well-known vitamin and cofactor therapies to the latest gene-and cell-based treatments.
To make sense of so much information, they grouped their findings into themes, ranging from long-used “mito-cocktail” supplements to exciting new areas such as boosting NAD+ levels, regulating cell-energy pathways (like mTOR), and developing gene therapies. By looking closely at both the successes and the setbacks, the authors highlight which treatments are showing real promise, which still need more study, and what lessons can guide future breakthroughs.
What did they find?
1. Current therapies
Right now, there’s no single cure for mitochondrial disease, so most treatments focus on easing symptoms, supporting energy production, and improving quality of life. However, for a few specific mitochondrial conditions, where doctors understand the exact chemical pathway that’s disrupted, certain vitamins and cofactors can make a measurable difference.
- Coenzyme Q10 (CoQ10): This molecule helps move electrons inside mitochondria, a key step in producing energy. In people with primary CoQ10 deficiency, whose bodies don’t make enough CoQ10, taking supplements can improve kidney and nerve function. Results vary, though, since CoQ10 doesn’t always reach the brain efficiently.
-
Thiamine (Vitamin B1): Helps enzymes that convert food into energy. When taken early, it can improve neurological symptoms in thiamine-responsive basal ganglia disease and some forms of pyruvate dehydrogenase complex deficiency
- Biotin (Vitamin B7): Needed for several enzymes that process fats and proteins. Lifelong biotin supplementation can prevent or reverse neurological and skin symptoms in people with biotinidase deficiency.
-
Riboflavin (Vitamin B2): Supports key mitochondrial enzymes. High-dose riboflavin has helped many people with ACAD9 deficiency and multiple acyl-CoA dehydrogenase deficiency regain strength and reduce fatigue..
Many people with mitochondrial disease also take nutritional supplements, often referred to as a “mitochondrial cocktail.” While the scientific evidence for their benefit is mixed, these supplements are generally safe and sometimes help with energy and stamina.
2. Emerging and experimental therapies
Researchers around the world are testing a variety of new treatments aimed at fixing or compensating for mitochondrial malfunction. Here are some of the most promising areas of discovery:
- Dietary approaches: High-fat, low-carbohydrate ketogenic diets and specialized fats such as triheptanoin may give cells an alternate energy source, helping reduce seizures or muscle weakness in certain conditions. Because these diets can sometimes cause side effects, they must be used with medical guidance.
- Stimulating mitochondrial growth: Some drugs, like bezafibrate, REN001, and omaveloxolone try to “switch on” the body’s own pathways that make and maintain mitochondria. Early studies show improvements in some cellular markers and mild symptom relief, though large-scale benefits have yet to be proven.
-
Restoring NAD⁺ balance: NAD⁺ is a molecule essential for energy production, and levels can drop in mitochondrial disease. Supplements such asnicotinamide riboside, nicotinamide mononucleotide, and KL1333 aim to restore these levels. Early trials suggest they may boost energy metabolism and reduce fatigue.
-
Antioxidant therapies: Because damaged mitochondria produce harmful reactive oxygen species (ROS), antioxidants can help limit that damage. Idebenone, vatiquinone (EPI-743), and sonlicromanol (KH176) are being tested for their ability to protect cells and support energy production. Idebenone has already shown benefit for vision in some people with Leber hereditary optic neuropathy.
-
Supporting blood flow and oxygen delivery: In certain mitochondrial syndromes like MELAS, supplements such as L-arginine and L-citrullinemay help widen blood vessels, improving circulation and reducing the risk of “stroke-like” episodes.
-
Modulating energy-sensing pathways: Drugs that act on the mTOR pathway (like rapamycin and everolimus) are showing benefits in laboratory models by reducing inflammation and improving energy balance.
-
Protecting mitochondrial structure: Elamipretide (SS-31) helps stabilize the membranes that hold mitochondria together, protecting them from damage. Some clinical studies show better muscle function and less fatigue, while others found only modest changes, highlighting the complexity of these conditions.
- Nucleoside replacement: In a few rare forms of mitochondrial DNA depletion (such as TK2 deficiency), therapy with building-block molecules called deoxynucleosides has helped restore mitochondrial DNA and improve survival.
-
Gene Therapies: Researchers are also exploring gene therapies that target the faulty gene itself. The majory of these approaches are experimental and are still early in development
In total, more than 30 clinical trials around the world are now testing therapies like these. None are yet curative, but the variety and sophistication of approaches reflect remarkable momentum. The field is moving from managing symptoms to targeting the root causes of mitochondrial dysfunction, an extraordinary step forward for patients, families, and researchers alike.
What does this mean for mitochondrial disease research?
This review marks an exciting turning point for mitochondrial medicine. For many years, research focused mainly on diagnosing and describing how mitochondrial diseases work. Now, the field is moving beyond understanding the problem, scientists are testing real treatments designed to fix it.
The authors emphasize that the road ahead still requires close teamwork across the globe. Researchers need better tools to study these diseases, including reliable biomarkers that show how the body responds to treatment, and agreed-upon outcome measures that make it easier to compare results between studies. Creating stronger animal models will also help scientists test therapies safely before they reach patients.
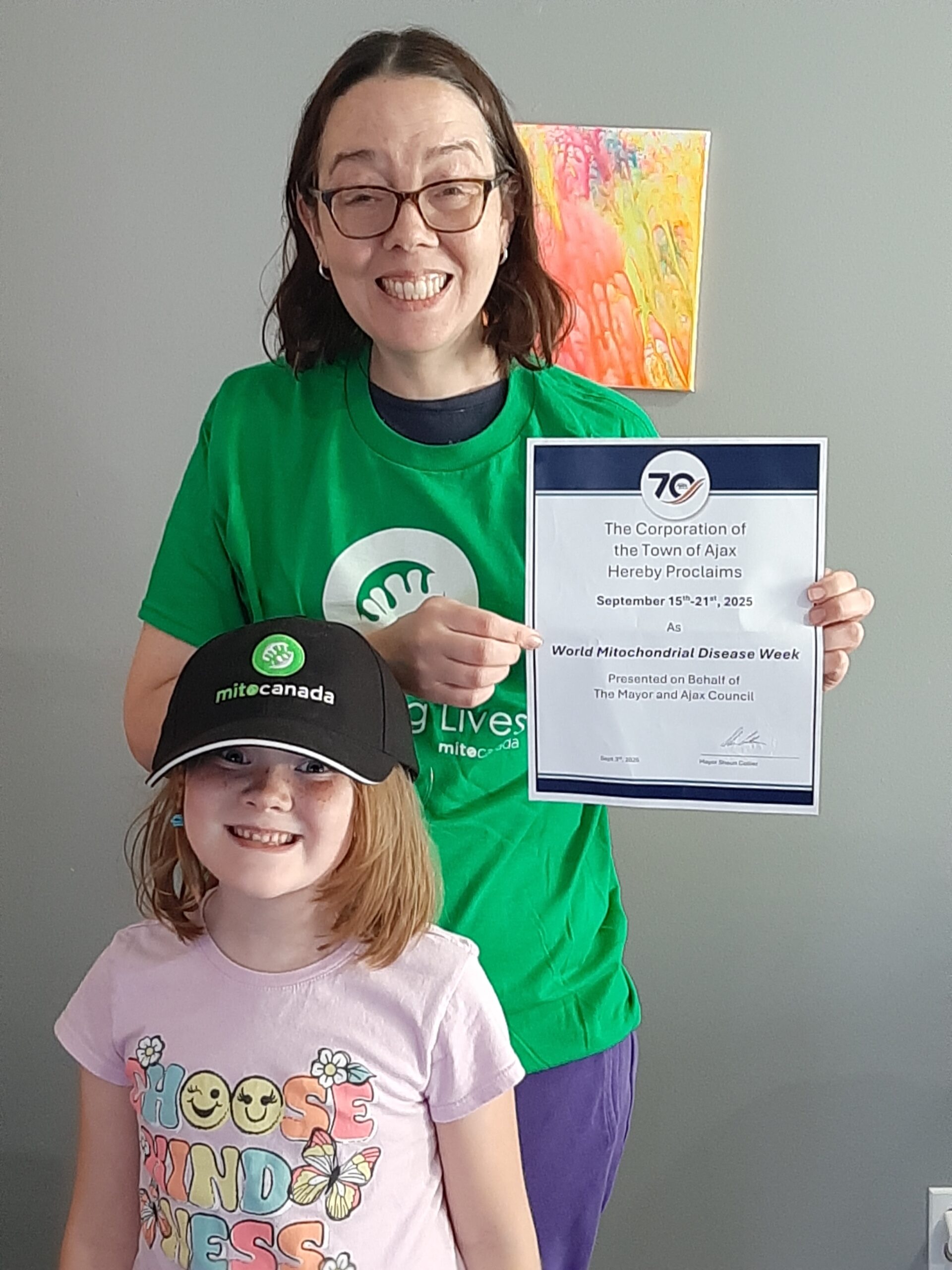
Just as important, progress will depend on collaboration, not only between scientists and clinicians, but also with patients, families, and advocacy organizations, like MitoCanada. Well-organized patient registries and international trial networks are key to making rare disease research faster, more efficient, and more inclusive. By working together, the global mito community is transforming years of discovery into a future filled with real treatment possibilities
The research in simple terms
This paper brings together everything scientists currently know about treating mitochondrial disease, from long-used vitamins and dietary strategies to the newest molecular and gene-based therapies being tested in clinics today. It highlights just how far the field has come since the first mitochondrial disorders were described in the 1960s.
While there’s still no single cure, the pace of progress is accelerating. Researchers are learning from both successes and setbacks, building on decades of discovery to design smarter, more targeted therapies. Just as importantly, the paper reflects the growing collaboration among scientists, clinicians, patients, and families, all working together to transform complex research into meaningful, real-world care.
At its heart, this is a story of perseverance and partnership: of a community united by determination to change what’s possible for people living with mitochondrial disease.
Why this matters to the MitoCommunity?
For those living with mitochondrial disease, and for everyone who supports them, this research represents hope backed by evidence. It shows that the global mito community is moving forward together: researchers exploring new frontiers, clinicians testing innovative treatments, and patient advocates ensuring that lived experiences shape every step of progress.
Each study like this adds another piece to the puzzle, helping to build a clearer picture of how to repair, protect, and strengthen the body’s energy-producing cells. These discoveries don’t just aim to extend life, they strive to improve how people live day to day, enhancing energy, independence, and connection.
The paper also reminds us how vital community participation is. Joining registries, contributing to research, and sharing personal stories all help guide future priorities and accelerate breakthroughs. And for donors and partners, it underscores a powerful truth: every investment in mitochondrial research moves us closer to a world where all lives are powered by healthy mitochondria.
Acknowledgment
The authors’ work reflects the incredible progress being made through collaboration across continents, disciplines, and generations of researchers. Their dedication not only advances the science of mitochondrial medicine but also fuels hope for families around the world. Every study like this brings us one step closer to a future where mitochondrial disease can be better understood, treated, and ultimately prevented.
This MitoInsights was reviewed and approved by a member of or members of this publications authorship.
Explore the orginial publication or download our layperson article today:
Do you have a question about this article? If so, we’d like to hear from you. Please send us an email!