Ground-breaking research that will prevent the devastating onset of mitochondrial disease and improve the lives of those already afflicted is urgently needed.
We need to bring together the brightest minds across the globe to develop better solutions for supporting the MitoCommunity. Excellence in health research is a recognized strength in Canada. We are known globally for the rigour and success of our clinical trials.
MitoCanada is supporting incredible scientists. We invite you to get to know them and their work.
Discovery Profile: Jessika Royea, PhD
MitoCanada partners with MITO2i to fund mitochondrial research that could introduce new therapies for Alzheimer’s disease Alzheimer’s disease [...]
Discovery Profile: Dr. Aneal Khan
MitoCanada funds research to advance Rapid Diagnosis of Mitochondrial Disease: Reducing diagnostic timing from years to days through generation sequencing [...]
Discovery Profile: Dr. Mark Tarnopolsky
MitoCanada funds research to support the development of novel therapies to treat mitochondrial diseases Exerkines™are a recently [...]
Discovery Profile: Robert Screaton, PhD
MitoCanada partners with MITO2i to fund mitochondrial research that could introduce new therapies for breast cancer Breast cancer [...]
Discovery Profile: Laura Rosella, PhD, MHSc
MitoCanada partners with MITO2i to fund an innovation grant to explain the health-system impact of mito disease and psychiatric conditions [...]
Discovery Profile: Dr. Ingrid Tein
MitoCanada partners with MITO2i fund mitochondrial research that could improve quality of life for those with autism spectrum disorder [...]
MitoCanada has a strong history of supporting research in its quest to find solutions for those living with mitochondrial disease today. Some of the research programs we have helped fund as outlined below.
Past Grants Awarded
Award Description: Sideroblastic Anemia With B-Cell Immunodeficiency, Periodic Fevers, And Developmental Delay (SIFD) Research Project
Grant amount: $53,000 over two (2) years.
Investigators: Martin Holcik, Urszula Liwak-Muir; Turaya Naas; Quinlan Wylie, Hanna Ludwig , Ribal Kattini, Chloe Campbell, Brianna Rino, Romanah Ahmed, Megan Williams, and Angelo Slade*
Research study:
Sideroblastic Anemia With B-Cell Immunodeficiency, Periodic Fevers, And Developmental Delay (SIFD) Research Project.
This research project aimed to understand the molecular mechanism of why mutations in a gene called TRNT1 cause this rare but devastating mitochondrial disease. TRNT1 is an essential enzyme that modifies all tRNAs in a cell; mature tRNAs are, in turn, required for the proper synthesis of all cellular proteins. In particular, the study focused on one aspect of SIFD pathology; the fact that the patient-derived cells are sensitive to oxidative stress. The working hypothesis was that TRNT1 deficiency results in reduced ability to repair tRNA termini and thus increased susceptibility to oxidative stress (and perhaps other stresses as well), thus contributing to the broad phenotype seen in SIFD patients.
The study identified several downstream proteins that are differentially expressed in patient cells. Researchers have further noted that the same proteins are differentially expressed in tissues derived from a mouse model of TRNT1.
This research study providing training for ten (10) trainees, two (2) manuscripts have been published and two (2) are currently being prepared.
*Trainees: Urszula Liwak-Muir (postdoctoral fellow; CHEO RI); Turaya Naas (postdoctoral fellow; CHEO RI); Quinlan Wylie (undergraduate student, CHEO RI), Hanna Ludwig (undergraduate student, CHEO RI), Ribal Kattini (undergraduate student, Carleton), Chloe Campbell (undergraduate student, Carleton), Brianna Rino (undergraduate student, Carleton), Romanah Ahmed (undergraduate student, Carleton), Megan Williams (undergraduate student Carleton), and Angelo Slade (Ph.D. student, Carleton)
Funding details: $53,686.81 per year for 2 years .
 Award: Administration of Human Mesenchymal Stem Cells as a Treatment for Mitochondrial Dysfunction.
Award: Administration of Human Mesenchymal Stem Cells as a Treatment for Mitochondrial Dysfunction.
Grant amount: $195,000 over three (3) years
Investigators: Chris Newell, Dr. Jane Shearer, Ph.D., Dr. Aneal Khan MSc, MD, FRCPC, FCCMG
Research Study: Mitochondria are the energy powerhouses of the cell, with the ability to generate a continual source of ATP to support basic metabolic function. Mitochondrial diseases are pathogenic genetic disorders, affecting ~1/3500-5000 individuals, with less than 50% of children surviving to adulthood. There is no current effective treatment or cure for mitochondrial disease. Mesenchymal stem cells (MSC) are multipotent cells capable of differentiating into various cell types. Their ability to target, modulate, regenerate and repair tissue has resulted in their use in multiple disease states during clinical practice.
As such, stem cell research as it relates to regenerating compromised tissue has exploded with experimental and clinical investigations reporting exciting therapeutic potential. Recent work from our laboratory and others has demonstrated that MSCs work in part by partial fusion, transferring intact mitochondria from cells to injured host tissue, altering host mitochondrial gene expression, enhancing metabolic capacity and reducing aberrant reactive oxygen species (ROS) production. All of these mechanisms have the potential to benefit host metabolic function including ATP generation. However, the rates of cell engraftment into host tissues is extremely low with less than 5% of cells surviving 24 h post transplantation. Our laboratory has shown that dietary manipulation (high-fat feeding) promotes MSC cell engraftment in various tissues. This discovery has tremendous potential to further our understanding of the factors that promote MSC cell homing and their impact on metabolism. Dietary manipulation is also a front-line treatment for certain mitochondrial diseases.
SPECIFIC OBJECTIVES. The overarching goal of my thesis is to use MSC as a tool to influence metabolism and treat mitochondrial dysfunction. Data garnered from the thesis will examine the efficiency, functionality and longevity of mitochondria transferred from MSC to the host in health and disease. Specific objectives are as follows:
-
-
- To determine the specific mechanisms by which MSC alter cellular bioenergetics and mitochondrial function.
- To utilize dietary manipulation to promote cell engraftment in host tissues.
- Examine the therapeutic potential of MSC in a model of mitochondrial disease.
-
OVERALL HYPOTHESIS. Stem cell therapy presents a novel modality for the treatment of mitochondrial disease. The overall hypothesis is that MSC therapy enhances mitochondrial oxidative phosphorylation (OXPHOS), gene expression and reactive oxygen species (ROS) scavenging capacity in the liver. This is accomplished, by increasing the density of functional mitochondria in the treatment animals. As a result, animals undergoing MSC treatment will possess increased mitochondrial function, with evidence of mitochondrial transfer from MSC.
Levels of cell engraftment and mitochondrial transfer will be greatest in animals with mitochondrial dysfunction as well as those experiencing metabolic stress induced by a ketogenic diet. Funding details: $105,000 (PH.D. Scholarship) with matching funds of $30,000/yr from Alberta Innovates for a total of $195,000 over three (3) years.
 Award Description: AMP-Activated Protein Kinase (AMPK) Activation for the Treatment of Mitochondrial Disease.
Award Description: AMP-Activated Protein Kinase (AMPK) Activation for the Treatment of Mitochondrial Disease.
Grant amount: $210,000 over two (2) years.
Investigators: Alexander Green, M.Sc. (Ph.D. Candidate); Mark Tarnopolsky, M.D., Ph.D., FRCP(C) (supervisor), Neuromuscular and Neurometabolic Clinic, McMaster University Medical Center and Dr. Gregory Steinberg, Ph.D.
Research study:
AMP-Activated Protein Kinase (AMPK) is an important energy-sensing enzyme. Normally, AMPK is endogenously activated under energy stress conditions by upstream kinases and direct binding of AMP. When active, AMPK activates pathways to limit energy use and increase energy-generating capacity in the cell. AMPK can facilitate this by increasing mitochondrial content and eliminating dysfunctional mitochondria. Novel therapies could be used to correct mitochondrial dysfunction in mitochondrial disease.
Funding details:
$35,000 per year for 2 years with matching funds from the Canadian Institute of Health Research (CIHR) Small Health Partnership Program (SHOPP) for a total award of $210,000 over the 3 years.
 Award Description: Using a novel and unique assay to screen small compound libraries for drug candidates to enhance mitochondrial function by improving ubiquinone-dependent respiratory chain function.
Award Description: Using a novel and unique assay to screen small compound libraries for drug candidates to enhance mitochondrial function by improving ubiquinone-dependent respiratory chain function.
Grant amount: $45,000 over one (1) year.
Investigators: Dr. Siegfried Hekimi, Ph.D, Department of Biology, McGill University, Montreal, Canada
Research study:
Mitochondrial diseases are often devastating conditions in which the energy generating function of mitochondria is impaired by mutations. One type of defect that leads to such impairment is when the organism is unable to synthesize enough ubiquinone (also called Co-enzyme Q, or CoQ10). In addition, probably because ubiquinone is synthesized in mitochondria, diseased mitochondria become less able to synthesize enough ubiquinone, which aggravates their condition. Unfortunately, simply providing patients with ubiquinone has only minimal effects on their health, probably because exogenous ubiquinone is poorly absorbed by most organs of the body. We have studied the biosynthesis of ubiquinone in a number of organisms, including mice. In particular, we have developed lines of cultured cells that are unable to make ubiquinone but are still able to grow as long as they are provided with glucose, which they can use for sufficient energy production in ways that don’t rely on mitochondrial function, which is defective because of the lack of ubiquinone. These cells die quickly in the absence of glucose but can be rescued if provided with added ubiquinone.
With the grant received from the MitoCanada Foundation we purchased and used compound libraries to search for drugs that can rescue or alleviate energy generation defects in UQ-deficient cells. Such drugs could act by boosting residual ubiquinone synthesis, by partially replacing ubiquinone for its function in mitochondria, by increasing the activity or the efficacy of residual endogenous ubiquinone, or even by boosting mitochondrial energy production in the absence of ubiquinone. Our screen has now already identified a number of compounds that prevent the death of the ubiquinone deficient cells. We are currently doing experiments to understand how these drugs act to produce their beneficial effects. We have previously developed a mouse strain which gradually loses ubiquinone from its mitochondria and becomes more and more sick in consequence. In the long term we will be able to test our most promising drug candidates on these mice and thus determine how much they might be able to help patients.
 Award: Calgary Next Generation DNA Sequencing Method for Mitochondrial Disease Diagnosis
Award: Calgary Next Generation DNA Sequencing Method for Mitochondrial Disease Diagnosis
Grant amount:$100,000 over three (3) years
Investigators: Dr. Aneal Khan, MSc, MD, FRCPC, FCCMG
Research study: Mitochondrial Disease in children using the Next Generation sequencing method (NGS). Mitochondrial disease causes abnormal function of the heart, brain, liver and muscles leading to poor development, strokes, multiple body dysfunctions and a shortened lifespan. Mitochondrial disease affects 1 in 5000 people. More than 1,000 genes are involved in mitochondrial function and previous methods of diagnosis involved invasive tissue biopsy, could only test a handful of genes, put patients at risk for procedural complications and could only make a diagnosis in a small number of cases. However, only about 20 – 25% of cases are diagnosed using traditional methods of tissue biopsy, biochemical analysis and candidate gene sequencing.
The NGS Project is a clinical platform using state-of-the-art technology for diagnosing Mitochondrial Disease and is the first of its kind in Alberta and Canada. NGS does not require painful and risky tissue biopsies and can be performed on DNA obtained from either a blood test or a cheek swab. The uniqueness of the project at Alberta Children’s Hospital aims to bring this technology to the bedside and make it easy to use by doctors who have patients with diseases for which a diagnosis has been elusive. By making a diagnosis of Mitochondrial Disease, doctors can make more precise decisions about treatment rather than wait the months or years to obtain an answer using traditional methods. With funding provided in part from MitoCanada, the group set out to analyze the exomes of 30 Albertan patients with unsolved cases of mitochondrial disease. Read the data presented on 12 pilot cases and the protocol recommended for 30 additional undiagnosed cases. Read more…
The impact of NGS in the lives of patients with Mitochondrial Disease cannot be overstated. As an example, from the 2012 grant from the CIBC, Dr. Khan recently identified a gene causing Mitochondrial Disease in an 8 year-old girl who has waited her entire life to find a diagnosis for a liver condition from which she nearly died at 4 months of age. It was not known whether the complications would lead to more medical problems in the future or what the future held for her. The NGS data identified a gene which has been shown to cause the same liver problems in infancy but most children gradually improved over time which means the prospects for this child to have a long term recovery are very good and she does not need to have another liver biopsy. In other patients, some of them were thought to have multiple sclerosis has been found to have a gene mutation causing Mitochondrial Disease. In another family, who had one child die of a severe undiagnosed disease and a second child also showing the same deterioration, a gene appears to have been identified that might provide a diagnosis and an easier method to diagnose the disease in other children or in future pregnancies.
Dr. Khan recognized the need for a different approach to the early diagnosis of rare genetic and metabolic diseases in Calgary. Driven by the desire to see a more innovative and faster process for patient screening, Dr. Khan saw an opportunity to open a private research facility geared towards advancing the diagnostics of rare genetic and inherited metabolic disorders. In January 2016, he opened the Metabolics And Genetics In Calgary (M.A.G.I.C.) Clinic which functions as Dr. Khan’s off-site research office, where his team conducts study procedures and recruitment from research protocols from the University of Calgary. The funding from MitoCanada was foundational in helping found this clinic startup, which offers free DNA testing (Mito-FIND) for patients showing signs and/or symptoms of mitochondrial disease as determined by their physician. More information here: magiccalgary.ca
Funding details: $100,000 in funding over three years. The Alberta Children’s Hospital Foundation provided $50,000 in matching funds.
 Award Description: Exome & RNA sequencing as a molecular diagnostic tool for Infantile Mitochondrial Diseases.
Award Description: Exome & RNA sequencing as a molecular diagnostic tool for Infantile Mitochondrial Diseases.
Grant amount: $45,000 over two (2) years.
Investigators: Eric A. Shoubridge(1), Isabelle Thiffault(2), Geneviève Bernard(3)
Research study: Exome & RNA sequencing as a molecular diagnostic tool for Infantile Mitochondrial Diseases; integration of effective computational strategy and functional analysis to characterize pathogenicity of variants in both mitochondrial DNA and nuclear genes encoding mitochondrial proteins.
Molecular diagnostic testing is commonly used to confirm clinical diagnoses of inherited mitochondrial diseases; however, sequence-based clinical diagnostics are often unavailable for individual genes or subgroups of diseases, and rarely provide the integration of both mitochondrial and nuclear exome data. Next-generation sequencing is a remarkable tool for the discovery of new disease genes, but remains challenging for interpreting DNA variations in individual patients. A growing number of genes are associated with infantile mitochondrial diseases, and as more than 1000 proteins participate in mitochondrial biology, we anticipate that many more disease-causing genes remain to be discovered. This research project is aimed at producing comprehensive diagnostic genetic tests for mitochondrial disorders, evaluating the impact of modifier genes on disease onset and severity, and investigating the pathogenesis of different mitochondrial disorders by functional analysis in cell lines obtained from patients. Funding details: $45,000 in funding for two years. (This project is also being supported by Children’s Mercy Hospital of Kansas City.)
 Award Description: An integrated mitochondrial diagnostics platform combining next-generation sequencing with respiratory studies in patient cells
Award Description: An integrated mitochondrial diagnostics platform combining next-generation sequencing with respiratory studies in patient cells
Grant amount: $87,000 over one (1) year.
Investigators: Matthew A. Lines MD MSc1, Dennis Bulman PhD1,2, Pranesh Chakraborty MD1,2, C. Anthony Rupar PhD3,4, Martin HolcikPhD2, Mary-Ellen Harper PhD5
Research study: Mitochondrial diseases represent a diverse group of genetic conditions that have traditionally proven difficult to diagnose, study, and treat due to their high degree of genetic heterogeneity. Although next-generation sequencing (NGS) easily permits the simultaneous sequencing of the >1000 known mitochondrial genes encoded across the nuclear and mitochondrial genomes, data interpretation is complicated by (i) the abundance of rare coding variants detected in any given individual, and (ii) a lack of knowledge regarding the functions and phenotypes of many mitochondrial genes. Early experience suggests that NGS-based testing will identify a known mitochondrial disease gene in up to ~25% of well selected probands; a further ~25% possess changes in novel candidate genes requiring functional assessment for validation of pathogenicity.
In order to enhance the access of Canadians with mitochondrial diseases to this crucial technology, we have assembled a translational working group comprised of experts in clinical metabolics, NGS-based disease gene identification, and mitochondrial physiology/bioenergetics. We propose a translational pilot study of mitochondrial diagnosis via NGS, backed by a panel of functional assays in patient cells to assess respiration, mitochondrial morphology and dynamics, and cellular redox status. The incorporation of functional information will allow us to (i) corroborate, refute and/or refine clinical hypotheses suggested by NGS data, and (ii) assess the in vitro efficacy of various substrates, cofactors, and drugs on intact patient cells. The methodological insights gained during the study will support the establishment of a permanent diagnostic resource, and the data (novel disease genes) will serve as a launching pad for several further basic science projects. Data regarding the in vitro drug / cofactor response profile of each specific condition (gene) will be used to frame further studies of tailored therapy.
Funding details: $32,000 in funding for one year. $55,000 matching provided by Children’s Hospital of Eastern Ontario
 Award: Frozen versus fresh: What type of muscle sample works best for the diagnosis of mitochondrial disease in a clinical laboratory?
Award: Frozen versus fresh: What type of muscle sample works best for the diagnosis of mitochondrial disease in a clinical laboratory?
Grant amount: $210,000 over three (3) year.
Investigators: Lauren MacNeil PhD 1, Murray Potter MD 1,3, Mark Tarnopolsky, MD, PhD2,4
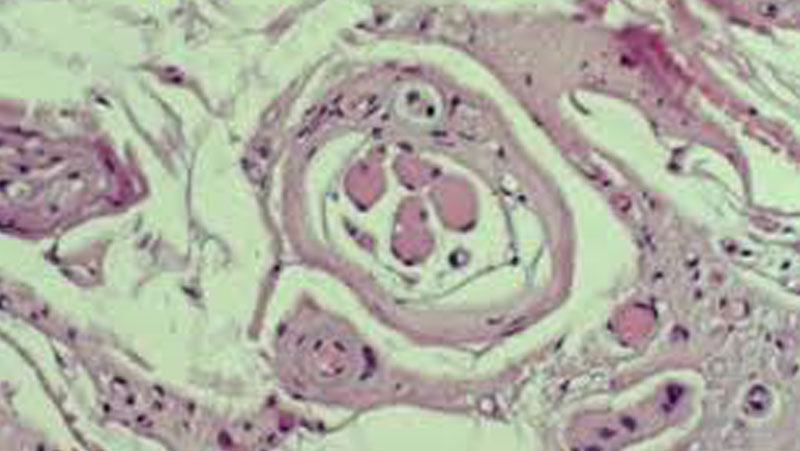
Research study: Diagnosis of mitochondrial disorder is achieved using biochemical testing of a muscle biopsy. Measurement of mitochondrial function is most accurate when it is done on fresh samples shortly after collection. However, many samples are collected in locations far from a diagnostic centre and must be frozen for storage/shipping. Freezing limits the types of analyses that can be done and can introduce factors that may alter the testing results and affect the ability to correctly detect mitochondrial dysfunction. Using muscle samples collected from adult participants with and without mitochondrial disease, we will compare high resolution respirometry and enzyme activity in fresh tissue to protein and enzyme activity in frozen tissue to determine if either method is superior.
Diagnosis of mitochondrial disorder is achieved using biochemical testing of a muscle biopsy. Measurement of mitochondrial function is most accurate when it is done on fresh samples shortly after collection. However, many samples are collected in locations far from a diagnostic centreand must be frozen for storage/shipping. Freezing limits the types of analyses that can be done and can introduce factors that may alter the testing results and affect the ability to correctly detect mitochondrial dysfunction. Using muscle samples collected from adult participants with and without mitochondrial disease, we will compare high resolution respirometry and enzyme activity in fresh tissue to protein and enzyme activity in frozen tissue to determine if either method is superior.
First, the investigators would like to thank MitoCanada for their generous funding of this research project and to let them know that there will be a long-term direct benefit that extends beyond the research. In large part due to this project, Dr. Lauren MacNeil was awarded one of only two coveted Ontario Ministry of Health and Long-term Care clinical genetics laboratory fellowship training scholarships this year. This scholarship will fund his training in the Canadian College of Medical Geneticists Biochemical Genetics training program at McMaster University for the next 2 years.
Since receiving funding for the above study we have recruited 34 participants with muscle disorders and 17 healthy males. Fresh muscle tissue was studied by high resolution respirometry and by enzyme activity. With sample collection just recently completed, enzyme assays on frozen tissue and data analyses are still ongoing; however we have made several early observations and will be reporting these findings at scientific meetings targeting inborn errors of metabolism and mitochondrial disease.
One report, which examines the stability of muscle samples after collection, will be made at the Garrod symposium this May in Vancouver. It is well known that, if not handled properly, the activity of respiratory chain complexes decrease over time, but the relative effect of sample handling on high resolution respirometry and enzyme activity assays is unknown. Our first report on this topic shares our observations on stability of muscle tissue stored for up to 1 week after excision for high resolution respirometry. Complex I activity was the first and most affected by time, falling by 45% in 24 h and reaching almost complete loss of function at 7 days. Complexes II and III were stable for 72 hours but by day 7 the activities were 44% and 50% lower, respectively. Complex IV was stable for 7 days. These results indicate that immediate measurement following excision would be imperative when reporting CI activity by high resolution respirometry.
Another observation will be reported this June at the United Mitochondrial Disease Foundation symposium in Washington. Several patients that participated in the study were found to have inclusion body myositis or polymyositis. These are inflammatory myopathies with muscle inflammation, muscular weakness and mitochondrial dysfunction. The high resolution respirometry in these patients showed a specific pattern: very low complex I and complex I + II flux, and a paradoxical increase in complex II flux to higherthan the complex I + II flux when complex I was inhibited. This implies that complex I impairs maximum complex II activity in these patients and hints at new areas to explore to understand and treat these disorders. Funding details: $210,000 in funding for three years with matching funding from the Canadian Institute of Health Research (CIHR) Small Health Partnership Program (SHOPP).
 Award: Strategies to Enhance Stem Cell Mediated Mitochondrial Transfer: Potential for the Treatment of Mitochondrial Disease.
Award: Strategies to Enhance Stem Cell Mediated Mitochondrial Transfer: Potential for the Treatment of Mitochondrial Disease.
Grant amount: $45,000 over one (1) year.
Investigators: Jane Shearer, Ph.D.; Jong Rho, MD; Steven Martin, MD; Aneal Khan, MD
Research study: This study examines the utility of cell-based therapy (stem cells) to alleviate symptoms associated with mitochondrial dysfunction. Stem cells are promising as they are able to reduce oxidative stress, alleviate inflammation and repair damaged tissues. Recent work also shows that they have the ability to transfer healthy mitochondria into host tissues. The goal of this research is to better understand this process and its potential clinical utility for the treatment of mitochondrial disease. The research team is unique as it combines expertise in mitochondrial disease, metabolic physiology, pediatric neurology and cell transplantation. With MitoCanada’ssupport we envision that our work will one day contribute to a cellular therapy for the treatment of mitochondrial disease.
Mitochondrial diseases are rare, but often devastating conditions with limited treatment options. The varied and often multifaceted nature of mitochondrial diseases requires an approach that will deliver or stimulate the proliferation of healthy mitochondria. A novel approach to accomplish this goal involves the administration of stem cells. Stem cells are early, multi-lineage cells (that can turn into many different cell types) and have immune privilege (not attacked by the immune system). This was the objective of our recent MitoCanada funded project ‘Strategies to enhance stem cell mediated mitochondrial transfer: potential for the treatment of mitochondrial disease’.
In this study, we show stem cells to target sites of mitochondrial dysfunction and to reduce a key hallmark feature associated with the disease, the production of excess reactive oxygen species. This reduction occurred 5 days post-administration, despite the finding that the majority of injected stem cells were no longer present in the liver, the key tissue of interest. This work was recently published. For more information, click here.
Going forward, we are trying to uncover ‘how’ this happens. While the laboratory initially hypothesized direct mitochondrial transfer from stem cells to host tissues, we are now showing stem cells to alter gene expression and mitochondrial networks, resulting in a shift away from mitochondrial metabolism to glycolytic means (from greek”glyco” meaning “sweet” and Greek “lysein” meaning “to break apart”). This shift results in a decreased dependence on mitochondria for energy production and reorganizes mitochondria to favor existing healthy mitochondria. To do this we are collaborating with Dr. Dustin Hitteland the National Children’s Hospital in Washington, DC to examine gene expression profiles of our samples. This will provide insight into how stem cells induce this switch. Data resulting from this study will enhance our understanding of cell-mediated regenerative mechanisms and the eventual development of a novel treatment for mitochondrial disease. Funding details: $45,000 in funding for one year.
 Award: Identification of Serum Factors Responsible for Systemic Mitochondrial Biogenesis
Award: Identification of Serum Factors Responsible for Systemic Mitochondrial Biogenesis
Grant amount: $41,000 over one (1) year
Investigators: Mark Tarnopolsky, M.D., Ph.D., FRCP(C); Justin Crane, M.Sc.; Adeel Safdar, Ph.D.; Arkan Abadi, Ph.D.
Research study: We have shown that long-term endurance exercise provided dramatic clinical protection in essentially all tissues in the body of a mouse model of mitochondrial disease (POLG1 mice). The protection extended to tissues not traditionally associated with exercise benefits including; gonads, skin, fur, eyes, lung and kidneys. This indicated that a systemic factor released in response to exercise was acting on distant tissues very much like a hormone. Our MitoCanada funded research will allow us to further identify these factors. The funding will partially support two major studies. The first is a cross-sectional study of 100 men and women between the ages of 20 and 86 with half being well trained athletes and half being sedentary controls. Analysis of mitochondrial function will be performed on cheek cells, skin, urine sediment (kidney cells) and blood to determine if systemic benefits that we saw in the mice also relate to humans.
The second aspect will be to try and identify the factors which confer systemic mitochondrial protection. To do this we will be culturing skin cells in the presence of serum from humans at rest and following exercise. First, we will identify the time of post-exercise where the serum has the beneficial effect on mitochondrial biogenesis and use that serum for proteomic analysis (identifying proteins) that are responsible for the effect. The long term goal is to identify a protein or proteins that could be injected in patients who cannot exercise to protect the mitochondria in multiple tissues. Overall, these results are likely to have significant implications for human aging, muscle physiology, exercise science and, most importantly, mitochondrial medicine.






